Antibody tests and our return to a more normal life
Time goes on, and the physical distancing measures successfully slow down the spread of the coronavirus. Now, we ask ourselves: how can we return to our work, friends, and overall normal life, and at the same time be safe? Fortunately, science has something up its sleeve. At the same time science warns us that one should not use it naively.
There are tests to show whether a person is currently infected (they are called RT-PCR-tests) or not. In addition, there are also tests to show whether a person is immune to COVID-2019. These tests are called antibody tests. These tests check for COVID-2019 antibodies – proteins that our immune system uses to neutralize viruses and other pathogens. A person recovered from an infection has antibodies against the virus and if the same viral particle enters the body next time, it normally gets quickly eradicated and does not cause a sickness. We do not know yet how long immunity to COVID-19 lasts, but scientists expect it to last at least several months, probably years. Therefore, people carrying antibodies against COVID-2019 will not get infected and will not spread the disease. Unlike PCR-tests, antibody instant-use kits can be mass-produced and used in a way similar to pregnancy tests. Such kits are being rapidly developed and will soon hit the market. Having antibodies is great. However, having a positive antibody test result, however, is not exactly the same.
While the tests are good, they are not perfect – as any other medical test. The test may detect antibodies although they are not present, or erroneously fail to detect them although the patient is immune. To get an approval for commercial use, the error rate of a test must be measured and reported. Let us look at an example. One approved for laboratory use in the US (Cellex qSARS-CoV-2 IgG/IgM Rapid Test) returns positive results for 93.8% of people, who indeed have antibodies. Correctly, 96.4% of people who do not have antibodies get a negative result in the test. At first sight, this looks good. However, let us see what would happen if we can deliver the test to literally everyone and decide to rely on the test alone.
Imagine a city of, say 1’000’000 people, such as Cologne. Imagine that 1% of the city inhabitants have been infected. The fraction of confirmed patients in Cologne is five times smaller but coronavirus is known to have many asymptomatic carriers and these don’t get into any statistics. Thus, the 1% is a rough inaccurate estimate, but not unreasonable. We use it here to illustrate how accuracy works and not to report the real clinical picture. Now, we test the whole city. Out of 10’000 people having antibodies, about 9’400 learn their correct status and can quit the quarantine without risk to themselves and others. Also, due to the test errors, in 600 people their antibodies will not be detected and they will be advised to stay home. So far, so good. However, a real problem comes from another type of test mistake. Remember, we do not know who is immune and screen the whole city. Out of 990’000 vulnerable people, more than 35’000 receive a positive test result by mistake. With 9’400 true positive outcomes and 35’000 mistakenly positive, only 21% of the positively tested people will actually be immune to the virus. In other words, four out of five positive tests will be erroneous in that city, even if the accuracy of the test itself far exceeds 90%.
From the perspective of the recipient of the positive test result, how reliable is the test prediction heavily depends on the fraction of infected people. In our imaginary city, we assumed that only 1% are infected. If the fraction of infected increases to 5% (50’000 people with antibodies), then approximately three out of five positive tests will be immune for real.
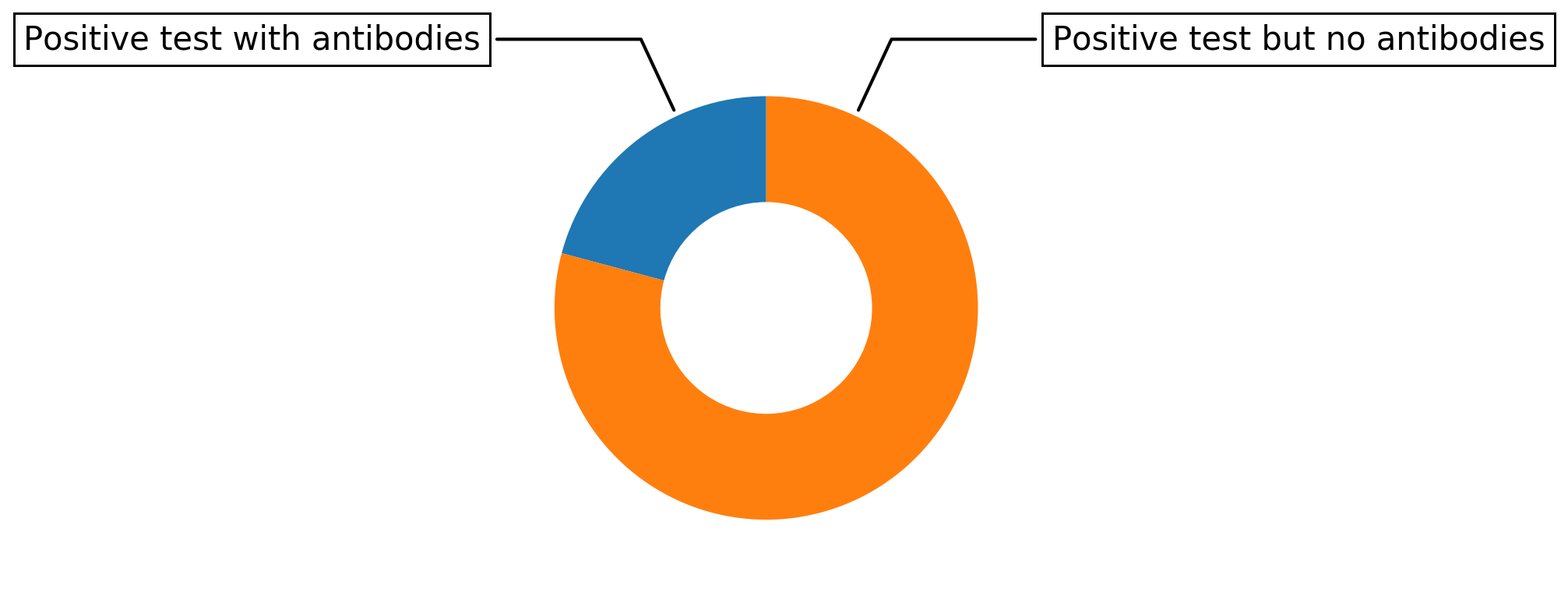
How much the positive outcome of a 96% specific test says about antibodies presence if 1% of the population has been infected. Only one out of five positively tested people has antibodies. All others are still vulnerable to the virus The less people were infected the less accurate is the test prediction.
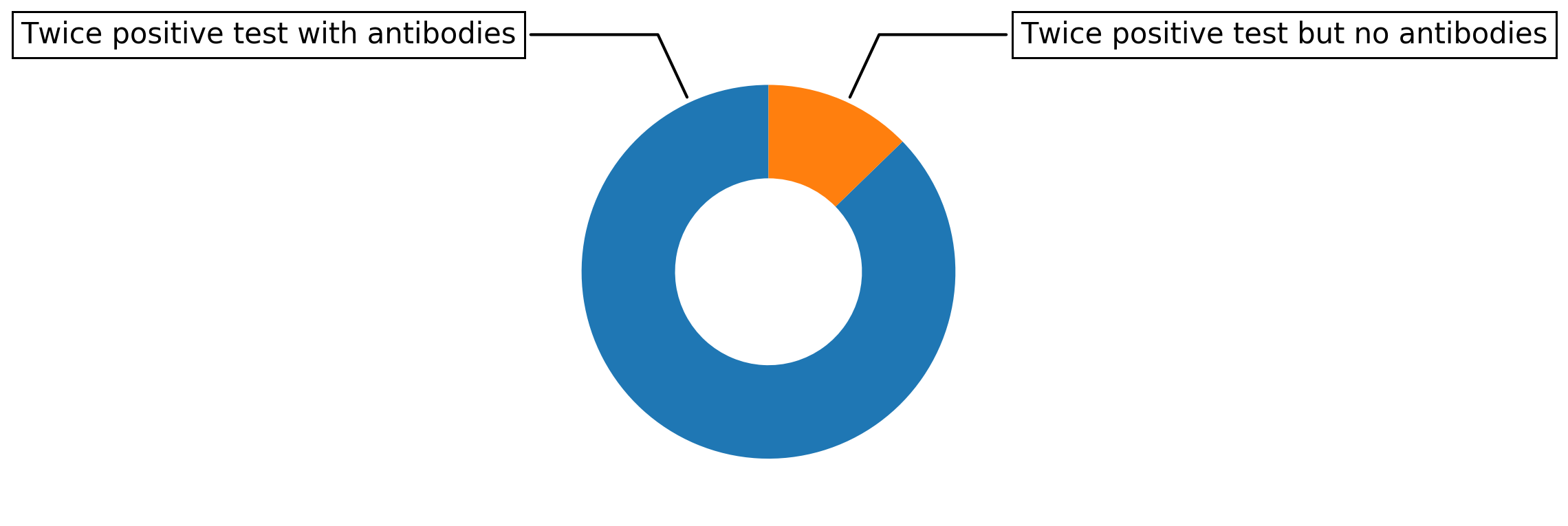
In clinics, many patients are actually sick and the test is expected to give accurate results. Outside clinics, however, the vast majority of people are not infected. This is why these tests cannot easily be used to test the whole population (or for spontaneously checking yourself). Still, antibody tests will be instrumental in our battle against the pandemic: once the tests are done repeatedly on the same cohort, the error reduces substantially: If we perform two independent (different!) tests in our scenario with 1% of the population being immune, 8800 people with positive test results will be truly immune and only about 1300 people with a positive result do not have antibodies to the virus. That means that a person who receives a positive test result can be almost 90% sure to be immune.
As a rule of thumb, an individual test result has to be handled with care as long as the incidence of the disease is small compared to the probability of an erroneously positive test result.
Twice performed, a 96% specific test results in 87% of double positive cases being actually immune. We assume 1% of the population has been infected, the less people were infected the less accurate is the test prediction.
Information about the test is taken from https://www.fda.gov/media/136625/download
Information about detected cases taken from https://www.statista.com/statistics/1105401/coronavirus-covid-19-cases-cities-districts-germany/
Authors: Dr. Yuriy Pichugin, Dr. Hildegard Uecker, Dr. Arne Traulsen.
